TAU achieves breakthrough in regenerative kidney medicine
Researchers grow human kidney organ cultures from tissue stem cells
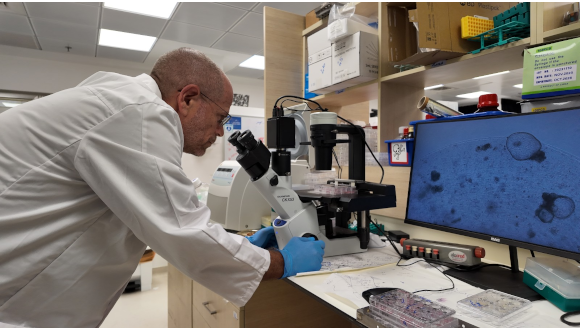
Support this researchResearchers from Tel Aviv University (TAU) and Sheba Medical Center have grown human kidney organoids, a synthetic 3D organ culture, from tissue stem cells in the laboratory, mirroring human fetal kidney development for the first time.
The current model has matured and stayed stable for over a half a year. Previous kidney organoids mimicking development broke down within four weeks. This allows long-term research and medical testing on kidney models.
The kidney grew and developed over months, allowing researchers to see the development of the organ in real time, isolate genes that lead to birth defects, develop new treatments in the field of regenerative medicine, and test the toxicity of drugs during pregnancy on fetal kidneys.
The groundbreaking study was led by Professor Benjamin Dekel, Director of TAU’s Sagol Center for Regenerative Medicine and Director of the Pediatric Nephrology Unit and the Stem Cell Research Institute at the Safra Children’s Hospital at Sheba Medical Center. The study was published on July 21, 2025, in The EMBO Journal.
The kidney is also the purest kidney organoid ever developed, with no cross contamination from stem cell development. Previous models using pluripotent stem cells would develop other cellular structures due to the unstable nature of the stem cells. The new organoid only expresses kidney cells, allowing for clear cause-and-effect experiments.
“Life begins with pluripotent stem cells, which can differentiate into any cell in the body,” explains Professor Dekel. “In the past, they were able to grow organoids by producing such general stem cells and sorting them into kidneys, but after about a month the kidney in culture died, and the process had to be started again.
“About a decade ago, my research group was able to isolate for the first time the human kidney tissue stem cells that are responsible for the growth of the developing organ. Now we have succeeded for the first time in growing a human kidney in the form of an organoid from the specific stem cells of the kidney, and this in parallel with the maturation process in the uterus that occurs until the 34th week of pregnancy.”
Researchers grow organoids in laboratory conditions to study organs in ways that are not possible in humans, but organoids derived from pluripotent stem cells often contain unwanted cells unrelated to the organ being studied that contaminate experiment data. Professor Dekel’s organoid grew from kidney tissue stem cells in a “clean” manner, since these stem cells differentiate exclusively into kidney tissue.
These cells developed into different types of kidney cells, and over half a year formed different tissues of the kidney, such as blood filter cells and kidney and urinary ducts, a process known as tubulogenesis.
“Growing the fetal kidney structures can shed new light on biological processes in general, and in particular on processes that lead to kidney diseases,” says Professor Dekel. “And indeed, when we selectively blocked a certain signaling pathways [in the organoid], we saw how it lead to a birth defect.
“We are actually seeing live how a developmental problem leads to kidney diseases that are seen in the clinic, which will enable the development of innovative treatments. We now have an essentially inexhaustible source of different kidney cells, and a better understanding of their different roles in kidney development and function.”
Also participating in the study were doctoral student Dr. Michael Namestannikov, a graduate of the Physician-Researcher track at TAU’s Gray Faculty of Medicine, and Dr. Osnat Cohen-Sontag, a research associate at Sheba Medical Center, as part of Professor Dekel’s research group.