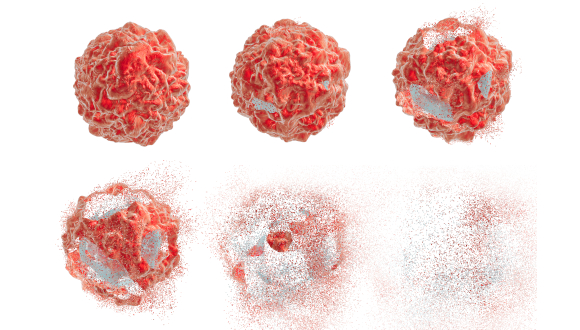
Combination of ultrasound and nanobubbles destroys cancerous tumors, TAU study finds
Technique allows for the removal of tumors without surgery
Support this researchA new technology developed at Tel Aviv University (TAU) makes it possible to destroy cancerous tumors in a targeted manner, via a combination of ultrasound and the injection of nanobubbles into the bloodstream. According to the research team, this latest technology enables the destruction of the tumor in a non-invasive manner, unlike invasive treatment methods or the injection of microbubbles into the tumor itself.
The study was conducted under the leadership of doctoral student Mike Bismuth from the lab of Dr. Tali Ilovitsh at TAU’s Department of Biomedical Engineering, in collaboration with Dr. Dov Hershkovitz of TAU’s Department of Pathology. Professor Agata Exner from Case Western Reserve University in Cleveland also participated in the study, which was published in August 2022 in the journal Nanoscale.
“Our new technology makes it possible, in a relatively simple way, to inject nanobubbles into the bloodstream, which then congregate in the area of the cancerous tumor,” Dr. Ilovitsh says. “After that, using a low-frequency ultrasound, we explode the nanobubbles, and thereby the tumor.”
The researchers explain that the prevalent method of cancer treatment today is surgical removal of the tumor, in combination with complementary treatments such as chemotherapy and immunotherapy. Therapeutic ultrasound to destroy the cancerous tumor is a non-invasive alternative to surgery, but this method has both advantages and disadvantages. On the one hand, it allows for localized and focused treatment; the use of high-intensity ultrasound can produce thermal or mechanical effects by delivering powerful acoustic energy to a focal point with high spatial-temporal precision. This method has been used to effectively treat solid tumors deep within in the body. Moreover, it makes it possible to treat patients who are unfit for tumor resection surgery. The disadvantage, however, is that the heat and high intensity of the ultrasound waves may damage the tissues near the tumor.
In the current study, Dr. Ilovitsh and her team sought to overcome this problem. In the experiment, which used an animal model, the researchers were able to destroy the tumor by injecting nanobubbles into the bloodstream (as opposed to the local injection of microbubbles into the tumor itself), in combination with low-frequency ultrasound waves, with minimal off-target effects.
“The combination of nanobubbles and low frequency ultrasound waves provides a more specific targeting of the area of the tumor, and reduces off-target toxicity,” Dr. Ilovitsh continues. “Applying the low frequency to the nanobubbles causes their extreme swelling and explosion, even at low pressures. This makes it possible to perform the mechanical destruction of the tumors at low-pressure thresholds. Our method has the advantages of ultrasound in that it is safe, cost-effective, and clinically available. In addition, the use of nanobubbles facilitates the targeting of tumors because they can be observed with the help of ultrasound imaging.”
Dr. Ilovitsh adds that the use of low-frequency ultrasound also increases the depth of penetration, minimizes distortion and attenuation, and enlarges the focal point. “This can help in the treatment of tumors that are located deep with the body, and in addition facilitate the treatment of larger tumor volumes. The experiment was conducted in a breast cancer tumor mouse model, but it is likely that the treatment will also be effective with other types of tumors, and in the future, also in humans.”
“Ramot, TAU’s tech transfer company, has applied for several patents to protect this technology and its application,” says Keren Primor Cohen, CEO of Ramot. “We believe in the commercial potential of this breakthrough technology in cancer treatment, and we are in contact with several leading companies in Israel and abroad to promote it.”