TAU researchers engineer human spinal cord implants for treating paralysis
Scientific breakthrough may enable people with paralysis to walk again
Support this researchResearchers from the Sagol Center for Regenerative Biotechnology at Tel Aviv University (TAU) have engineered 3D human spinal cord tissues and implanted them in laboratory animal models with long-term chronic paralysis. The encouraging result was an approximately 80% success rate in restoring walking abilities. Now the researchers are preparing for the next stage of the study: clinical trials in human patients. They hope that within a few years the engineered tissues will be implanted in paralyzed individuals enabling them to stand up and walk again.
The groundbreaking study was led by Professor Tal Dvir‘s research team at the Sagol Center for Regenerative Biotechnology, the Shmunis School of Biomedicine and Cancer Research, and the Department of Biomedical Engineering at TAU. The results of the study were published in the journal Advanced Science.
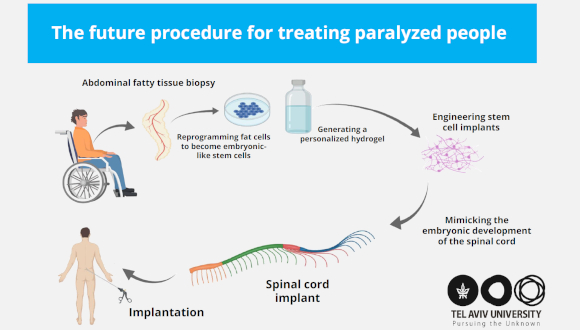
“Our technology is based on taking a small biopsy of belly fat tissue from the patient,” Professor Dvir explains. “This tissue, like all tissues in our body, consists of cells together with an extracellular matrix (comprising substances like collagens and sugars). After separating the cells from the extracellular matrix we used genetic engineering to reprogram the cells, reverting them to a state that resembles embryonic stem cells – cells capable of becoming any type of cell in the body.
“From the extracellular matrix we produced a personalized hydrogel, that would evoke no immune response or rejection after implantation. We then encapsulated the stem cells in the hydrogel and, in a process that mimics the embryonic development of the spinal cord, we turned the cells into 3D implants of neuronal networks containing motor neurons.”
The human spinal cord implants were then implanted in laboratory animal models, divided into two groups: those who had only recently been paralyzed (the acute model), and those who had been paralyzed a period equivalent to a year in human terms (the chronic model). Following the implantation, 100% of the lab models with acute paralysis and 80% of those with chronic paralysis regained their ability to walk.
“The model animals underwent a rapid rehabilitation process, at the end of which they could walk quite well,” Professor Dvir observes. “This is the first time that implanted engineered human tissues have generated recovery in an animal model for long-term chronic paralysis – which is the most relevant model for paralysis treatments in humans.
“There are millions of people around the world who are paralyzed due to spinal injury, and there is still no effective treatment for their condition. Individuals injured at a very young age are destined to sit in a wheelchair for the rest of their lives, bearing all the social, financial, and health-related costs of paralysis. Our goal is to produce personalized spinal cord implants for every paralyzed person, enabling regeneration of the damaged tissue with no risk of rejection.”
Professor Dvir teamed up with industry partners to establish Matricelf (matricelf.com) in 2019, which sought to develop the revolutionary organ engineering technology developed in his lab. The company applies Prof. Dvir’s approach with the aim of making spinal cord implant treatments commercially available for persons suffering from paralysis.
“We hope to reach the stage of clinical trials in humans within the next few years, and ultimately get these patients back on their feet,” Professor Dvir concludes. “Matricelf’s preclinical program has already been discussed with the FDA. Since we are proposing an advanced technology in regenerative medicine, and since at present there is no alternative for paralyzed patients, we have good reason to expect relatively rapid approval of our technology.”
The team at Professor Dvir’s lab includes PhD student Lior Wertheim, Dr. Reuven Edri, and Dr. Yona Goldshmit. Other contributors included Professor Irit Gat-Viks from the Shmunis School of Biomedicine and Cancer Research, Professor Yaniv Assaf from the Sagol School of Neuroscience, and Dr. Angela Ruban from the Steyer School of Health Professions, all at Tel Aviv University.